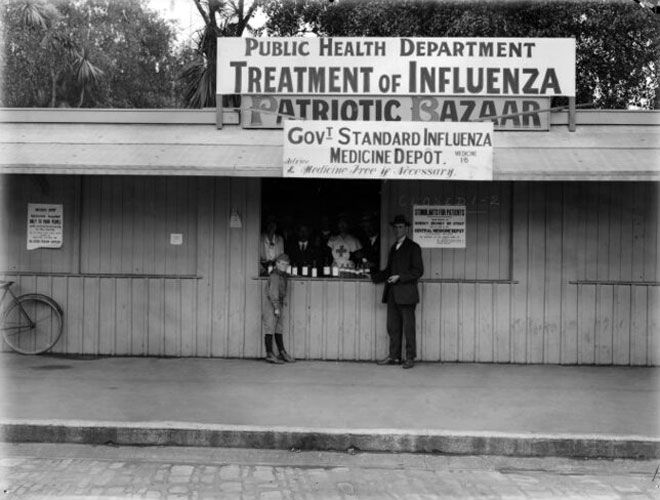
MCH Senior Historian Elizabeth Cox has been pondering the similarities and differences in New Zealand’s response to two pandemics – the 1918 flu, which was one of the defining events of the 20th century, and the COVID-19 pandemic in 2020, which while still unfolding is on course to be equally significant for the 21 century. Here are some of her preliminary thoughts.
The flu pandemic of 1918 (sometimes called the Spanish Flu) was New Zealand’s most devastating peacetime event, with 9000 deaths and 40% of the population infected. It followed on directly from the devastation of the First World War, so communities were already traumatised. You can read more about the flu pandemic in our NZHistory feature.
Historian Geoffrey Rice has written an interesting piece in which he discusses the differences and similarities between the 1918 and 2020 pandemics. He wrote this article in early March 2020, when the seriousness of the pandemic was just starting to become clear overseas, and we had only had one case. What a lot has changed since then!
Geoffrey is clear that ‘history never repeats’ – many features of this pandemic make it different from the 1918 experience. There are certainly some striking differences, but also some similarities, in the situation as it has developed so far.
Readiness and listening to early warnings
The timing of the 1918 flu meant that many doctors and nurses who might have been able to help the New Zealand community fight it were still overseas or had died. Many of the soldiers who returned to New Zealand while the pandemic was raging would not have been well, after strenuous war service. In 2020 we were more ready, with a better-resourced health system and plans for dealing with pandemics already prepared.
Furthermore, in 1918 New Zealand ignored the early warnings from overseas. In 2020, however, having watched what was happening elsewhere, and before a single death had occurred here, New Zealand adopted an early and increasingly strict lockdown policy – a decision that has so far kept the disease from spreading out of control.
Better communications
As you would expect, our communications now are better than they were then. Geoffrey Rice explains that the unreliable telegraph system in 1918 allowed the pandemic to get twice as bad in Wellington as it was in Christchurch because messages were slow to get through. Many local authorities were confused or didn’t follow instructions properly, which made things worse in some places.
This time, the system of Alert Levels instituted by the government has made it reasonably easy for people to understand what they need to do and what they can do. The Prime Minister and the Director-General of Health deliver clear messages at daily press conferences, and the Ministry of Health’s COVID-19 website has a lot of information.
Proper isolation
During the 1918 pandemic, many public facilities and businesses were shut, although unlike 2020 there was no general order to do so. Blue-collar workers in 1918 were not entitled to annual or sick leave so many kept working. Rice argues that this was a key reason for the higher male death rate with the flu pandemic. In 2020 the government provided billions of dollars in wage subsidies. Most large public events were cancelled in 1918, as has happened more systematically in 2020. Schools closed too, and with no online learning the holidays came early for children whose families stayed healthy.
Two big mistakes were made in 1918 which contributed greatly to the spread of influenza. The first was to allow Armistice Day celebrations to mark the end of the First World War, such as this event, attended by 8000 children in Christchurch. Armistice Day was 12 November 1918, by when a second, more serious strain of the influenza virus was well-established in New Zealand.
The second major mistake was the decision to gather people together, sometimes 50 or 60 at a time, and spray them with a gas, zinc sulfate, to try to make their lungs healthier. Geoffrey Rice says that the spray was medically useless – and by bringing people together, it would have actually spread the disease through communities. Listen to a man recalling what these ‘inhalation centres’ were like.
In 2020, the lockdown during Level 4 has meant that almost everyone has kept to their ‘bubbles’ and avoided gathering in public. There have been some exceptions, but the police have been vigilant in ensuring no large gatherings have been taking place.
Access to food
Something that is different now is access to food and medicine – with social distancing at supermarkets and pharmacies, and ‘contactless’ courier delivery services. Back in 1918, however, children’s groups such as the Scouts (shown below) were often used to deliver food to very sick people in their neighbourhoods.

Christchurch City Libraries, PhotoCD2 IMG0048
Scouts carrying baskets of food and medicine during influenza pandemic, 1918.
Listen also to this audio clip of the memories of a girl who was asked to deliver food to sick neighbours, riding around on her horse. Child delivery services are certainly not happening today!
The pandemics and Māori
Māori communities were devasted by the 1918 pandemic. The statistics were shocking. The death rate was more than eight times that for Pākehā. There were many reasons. One was that most Māori population at that time lived in rural areas, so they had lower immunity to colds and other minor respiratory ailments, and had largely avoided the mild first wave of the pandemic, which gave some immunity to those who contracted it. Geoffrey Rice also suggests that lower standards of housing, clothing and nourishment put Māori communities at greater risk.
There was also prejudice at the time, with Māori somehow blamed for the pandemic. While many Pākehā communities banded together, they sometimes left neighbouring hapū and marae to fend for themselves. Whina Cooper recalled the suffering at Panguru, Hokianga:
Everyone was sick, no one to help, they were dying one after the other. My father was very, very sick then.… He was the first to die.… I couldn't do anything for him. I remember we put him in a coffin, like a box. There were many others, you could see them on the roads, on the sledges, the ones that are able to drag them away, dragged them to the cemetery. No time for tangis.
As well as desolation, however, there were also tales of great bravery in Māori communities in 1918. On this page you can see some examples, including the remarkable story of Marion (Mereana) Hattaway, who led the battle against the disease in Te Kuiti at Te Tokanganui-a-noho Marae.
Today, understanding of the health inequities Māori face is much greater, although some Māori communities still feel that their health needs have not been sufficiently taken into account. This RadioNZ article reflects some of the concerns of Māori health leaders, particularly those of the Māori National Pandemic response group Te Rōpū Whakakaupapa Urutā, which includes primary care specialists, public health experts, doctors and nurses, and iwi leaders.
The Tūhoe iwi, who live in the Urewera area of the North Island, have been proactive in their response to COVID-19. They have set up their own pop-up testing centres for anyone concerned they may have the disease. They have also set up checkpoints on roads into the Urewera area, to stop non-essential travel, and engage with people, to explain the rules and encourage them to stay within their bubble. They hope to achieve the same outcome as in 1918, when the epidemic did not penetrate Te Urewera because Te Whāiti policeman Andy Grant banned all travel into the interior for several weeks.
Even during Level 3, when hunting will be allowed again in much of the country (under strict rules), Te Urewera Board (which manages Te Urewera and the Lake Waikaremoana Great Walk) has asked hunters to stay away from their area. . Only locals & essential services can legally access Te Urewera under Level 3.
Learning from our mistakes using history
After occupying German Samoa on the outbreak of the First World War, New Zealand was blamed for mishandling the 1918 influenza pandemic. Influenza arrived in Samoa on 7 November 1918, when the passenger and cargo ship Talune docked in Apia. The acting port officer was unaware that there was a severe epidemic at the ship's departure point, Auckland. As a result, he allowed passengers ashore, including six who were seriously ill with influenza. Within a week, influenza had spread throughout the main island of Upolu and the neighbouring island of Savai'i. An estimated 8500 Samoans – 22% of the population – died in the pandemic. There was famine in 1919 because crops hadn’t been planted when Samoa was in the grip of the pandemic.
Measles outbreak
The vulnerability of island nations such as Samoa to the introduction of highly contagious infectious diseases can be seen in the spread of the measles virus. Measles arrived for the first time in Samoa in 1893, aboard a ship from New Zealand. By year’s end, over 1,000 people (of a total population of 34,500 at that time) had died. More died the following year. Another outbreak in October 2019, via an infected passenger on a flight from Auckland, resulted in nearly 6,000 cases and 83 deaths by early 2020.In March 2020, as the threat posed by COVID-19 became apparent, Samoa, like New Zealand, imposed travel restrictions after announcing its first suspected case of coronavirus – a person who had arrived in the country from New Zealand. Anyone due to fly to Samoa for whatever reason was advised to cancel their trip. It was announced that Samoa’s border restrictions would be strengthened.
Historians are often useful in understanding how and why things happened in the past, but it isn’t often that they get to make a real-life difference to how many people survive in the future. The research Geoffrey Rice did on the 1918 pandemic has contributed to New Zealand’s Pandemic Plan, which is now the guiding document being used to fight the COVID-19 pandemic. Hopefully his work can help us come through the current pandemic. It will be interesting to see how quickly we return to what might be described as a ‘normal life’ or whether the experience of living and working in various stages of lockdown will change how we go about daily life.
Senior Historian Elizabeth Cox
More information:
- NZHistory feature The 1918 Influenza Pandemic
- Te Ara feature on Epidemics
- Geoffrey Rice, Black November: the 1918 influenza pandemic in New Zealand, 2nd edition, Canterbury University Press, Christchurch, 2005


Community contributions